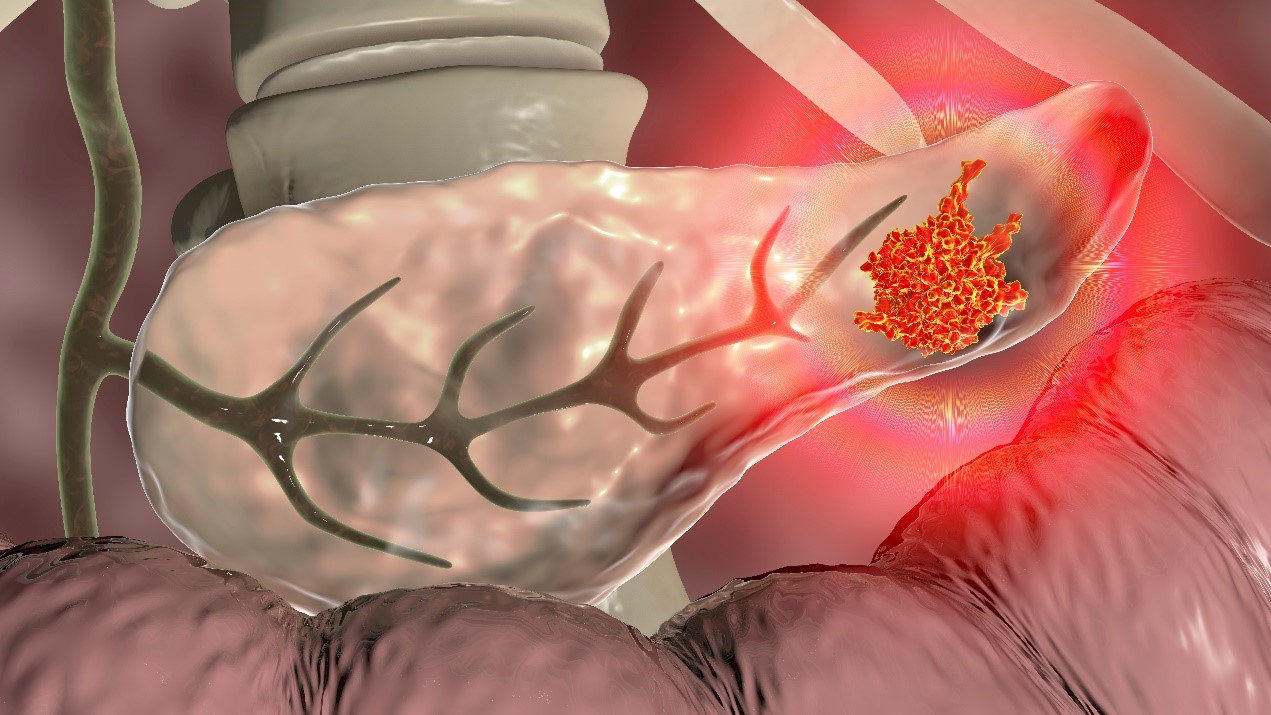
Pancreatic cancer develops when cells in the pancreas grow uncontrollably, often forming a malignant tumor.
This gland in the abdomen plays a crucial role in digestion and hormone production.
Common symptoms include
- Jaundice
- Abdominal and back pain
- Nausea
- Unexplained weight loss
but these typically appear in later stages.
Early detection is difficult, as tumors rarely show on initial imaging tests, often leading to late-stage diagnoses.
Diagnosis and Testing
Detecting pancreatic cancer early is challenging because the pancreas is positioned deep in the abdomen, making physical exams ineffective in the early stages.
When pancreatic cancer is suspected, doctors use a series of tests to diagnose and evaluate the disease.
These include advanced imaging techniques like
- CT scans
- MRIs
- Endoscopic ultrasounds
to visualize the tumour.
- Blood tests may detect tumour markers such as CA 19-9, which are elevated in many patients with pancreatic cancer.
- Genetic testing is also advisable for those with a family history of the disease to identify potential hereditary risks.
Treatment Options
Treatment strategies for pancreatic cancer depend on the tumour’s stage and location.
Options include:
- Surgery: This is the most effective treatment for resectable pancreatic cancer. Standard procedures include the Whipple procedure, which is used for tumours located in the head of the pancreas, and distal pancreatectomy for tumors in the tail.
- Chemotherapy and Radiation: These treatments may be used before surgery to shrink tumours or after to eliminate remaining cancer cells. They are also primary treatments when surgery isn’t an option.
- Targeted Therapy: These drugs specifically attack cancer cells with less damage to normal cells, and they are suitable for certain types of pancreatic cancer based on genetic factors.
Additionally, managing pain and digestive issues is critical, as the pancreas plays a vital role in digestion.
Prevention and Risk Management
While it’s impossible to prevent pancreatic cancer completely, you can reduce risk factors.
- Steering clear of tobacco
- Keeping a healthy weight
- Reducing exposure to harmful chemicals
can lower risk.
Regular medical check-ups are essential for those with a high risk of developing the disease, such as individuals with a family history of pancreatic cancer.
Living With Pancreatic Cancer
Managing life with pancreatic cancer involves both physical and emotional adjustments.
Patients should proactively collaborate with their doctors to grasp their treatment choices and possible side effects.
Joining support groups and seeking counselling can offer vital emotional and psychological support.
Additionally, it’s crucial to talk about ways to manage pain and make lifestyle changes that help control symptoms effectively.
For individuals at risk or diagnosed with pancreatic cancer, proactive communication with doctors is crucial to navigate this challenging journey. Staying informed and supported can help manage the condition more effectively and enhance quality of life.
Schedule regular check-ups and screenings to stay ahead in your fight against pancreatic cancer.