Urology
- Home
- Urology
Department of Urology
The recent development in medical science has been a very important one for the department of urology in view of the development of Laparoscopic urology surgery and Endo-urology. We take seriously our three-fold mission of academic excellence, hard work and research.
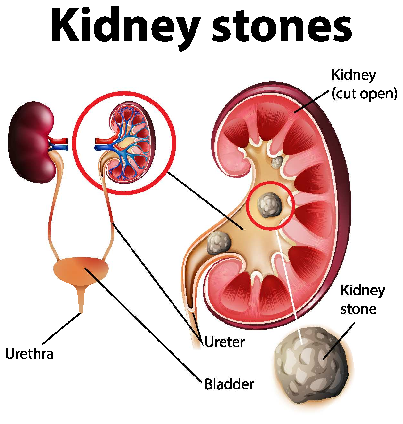
Stones (Kidney, ureter and bladder)
Kidney and ureteric stones form when substances that are normally dissolved in the urine concentrate together and aggregate into stones. They can cause severe pain in flank that radiates to groin (with associated dysuria or haematuria) and often require visits to the emergency room if stones are of larger size and obstruct the urinary tract. Studies have shown that patients who have a single symptomatic kidney stone are likely to have another if not treated within five years. Our goal is to provide the most advanced treatment for painful kidney stones and also long-term management strategies, such as dietary modification and medical management, to prevent stones from recurring.
According to Size of Stones:
A) Stones smaller than 4-5mm are usually treated conservatively with medications and advice to drink plenty of water.
B) Stones larger than 7-8mm need surgical intervention as unlikely to pass spontaneously.
C) Stone of 5-7mm are initially conservatively treated but if stones does not passes and there is persistent Urinary tract obstruction documented by hydroureteronephrosis then surgery is advised.
At LIGG, we specialize in minimally invasive surgery for kidney and ureteric stones, including ureteroscopic lithotripsy (URSL) and percutaneous stone removal in addition to lithotripsy (PCNL), which uses powerful shock waves to break up stones. These minimally invasive options lead to faster recovery time and improved patient outcomes.
Benign Prostatic Hyperplasia (BPH)
The main function of the prostate gland is to produce ejaculatory fluid. The prostate gland often enlarges with age, referred to as benign prostatic hyperplasia or BPH. This condition can cause symptoms such as difficulty emptying bladder, need to urinate frequently, straining, post urination dribbling or weak stream. These symptoms are referred to as lower urinary tract symptoms (LUTS) and occur because the gland is enlarged and blocking the flow of urine.BPH is a common condition, estimated to affect 50% of men in their 50s and up to 90% of men over age 80. In addition to increasing age, other risk factors include family history of BPH. BPH is not prostate cancer, although the conditions can exist together. BPH is a progressive disease and can result in bladder damage, infection or kidney damage. BPH symptoms can be treated with oral medications used to decrease the size of the prostate (5-alpha-reducatase inhibitors) or to relax the muscles of the prostate and bladder neck (alpha blockers). Procedures such as transurethral resection of the prostate (TURP) , Saline Bipolar TURP are routinely performed at LIGG for patients with Obstructive symptoms and high residual urine volume.
Hematuria (blood in urine)
Hematuria refers to the presence of blood in the urine. If the blood is visible it is called gross hematuria. Most men with hematuria do not have symptoms. Hematuria can originate from any site along the urinary tract, including the kidneys, ureters, bladder, prostate, or urethra. Hematuria has many causes, including vigorous exercise, sexual activity, viral illness, trauma/injury, or infection such as a urinary tract infection (UTI). More serious causes include kidney or bladder stones, cancer in the urinary tract, and many medical conditions particularly Tuberculosis (as its more common in India). Hematuria evaluation may include use of cystoscopy—looking inside the bladder with a thin, flexible telescope—to visualize the bladder, and imaging with CT or MRI to visualize the kidneys and ureters. Urine tests include cytology to look for cancer cells in urine and urine culture to rule out infection.
Urinary Tract Infection (UTI)
UTI is one of the most common reasons people visit their physician. Normal urine is sterile and contains no bacteria. Bacteria can enter through the urethra and invade the urinary tract lining and urine from nearby skin and rectal area. Women are more prone to UTI because they have shorter urethras. An estimated 40% of women and 12% of men will experience as least one symptomatic UTI during their lifetime. UTI is typically diagnosed based on medical history and confirmed with urinalysis with or without urine culture. Fevers and more severe pain may prompt greater workup such as computed tomography (CT scan) in order to image the kidneys. Most simple UTIs can be treated with a short course of oral antibiotics. Ways to avoid UTI include urinating after sexual intercourse, drinking normal amount of fluids to stay hydrated, and wiping from front to back when using bathroom (to prevent rectal bacteria from entering vagina or urethra).
Female Voiding Dysfunction
The lower urinary tract, which includes the bladder and urethra, allows for storage and timely expulsion of urine. Voiding dysfunction is a broad term, used to describe conditions where there is poor coordination between the bladder muscle and the urethra. This results in incomplete relaxation or overactivity of the pelvic floor muscles during voiding. Voiding dysfunction can manifest as a wide range of symptoms which can include difficulty in emptying bladder, urinary hesitancy, slow or weak urine stream, urinary urgency, urinary frequency or dribbling of urine. Voiding dysfunction can be due to nerve dysfunction, non-relaxing pelvic floor muscles or both. Voiding dysfunction is also classified as being caused by either underactivity of the bladder (detrusor) or outflow (urethra). Evaluation by a clinician may include tests, such as uroflowmetry, post-void residual and pressure flow studies. Treatment is individualized, depending on specific etiology. Possible treatments include pelvic floor therapy, intermittent self-catheterization, muscle relaxants or placement of a neuromodulation device. Specific conditions that fall within spectrum of female voiding dysfunction include Urinary Incontinence and Interstitial Cystitis.
Male Sexual and Reproductive Health
Following conditions are routinely treated at LIGG hospital by our Urologists -Erectile dysfunction (ED) , Hypogonadism (low testosterone), Male Infertility, Peyronie’s Disease, Prostatitis (male pelvic pain), Testicular Pain, Decreased Libido, Ejaculatory and Orgasmic Disorders
Trauma and Reconstruction
his involves management of Urinary Fistula Repair (UV Fistula, Vesico-vaginal fistula and Recto-vaginal Fistula), Genital Reconstruction (Hypospadias Surgery), Urethral Stricture, Urinary Incontinence and Urological Prosthetic Surgery